Pathology, Cognition, and Biomarkers: Comparing Parkinson’s & Alzheimer’s
Although Parkinson’s disease and Alzheimer’s disease are both common neurodegenerative disorders, their underlying biology, cognitive symptoms, and biomarker profiles differ in important ways. Understanding these distinctions helps clinicians better diagnose, monitor, and treat each condition, and sheds light on why patients experience such different symptoms.
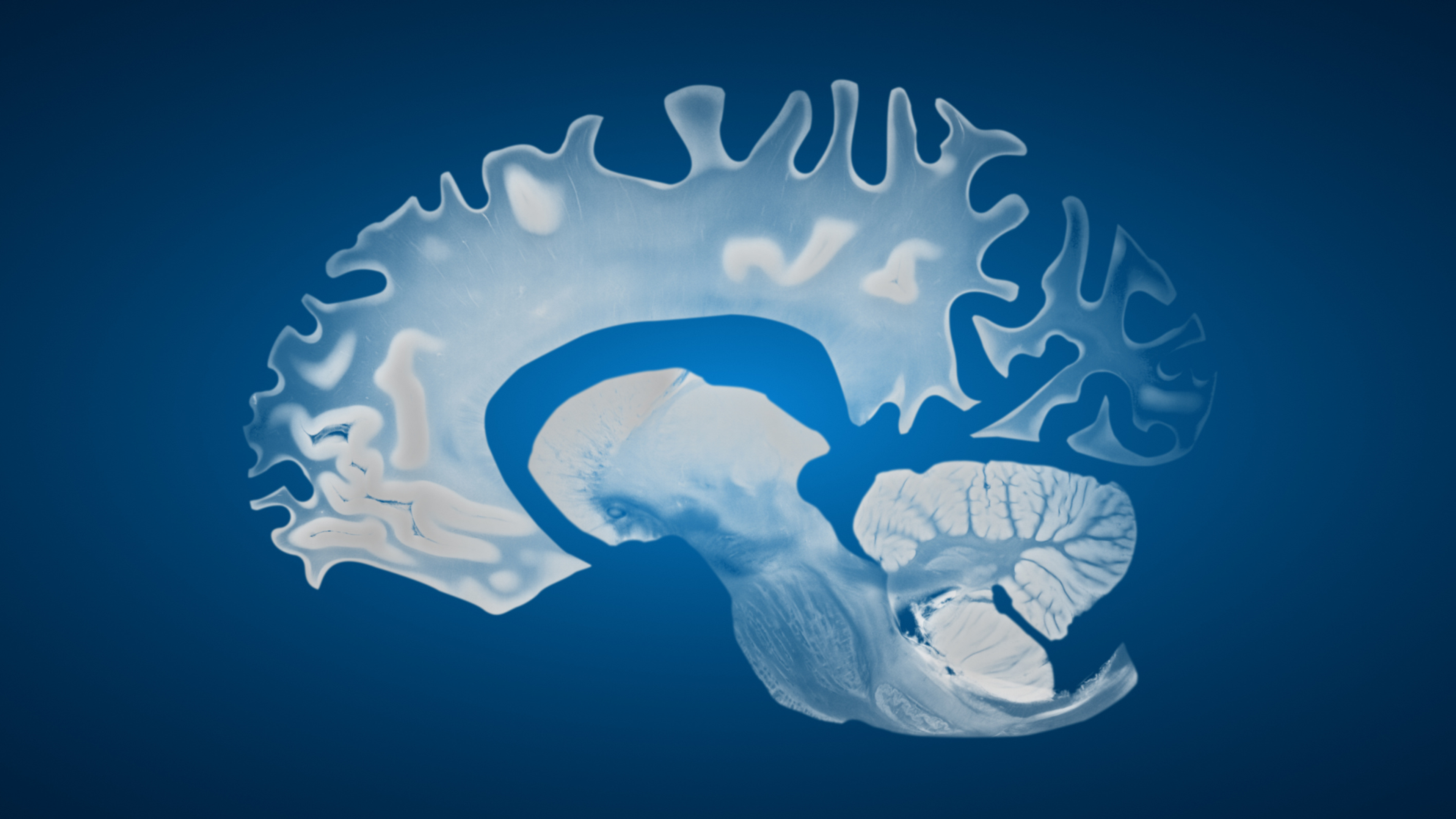
Dr. Jonathan Isaacson explains that “Parkinson's Disease and Alzheimer's disease present differently… and part of that is because of the pathophysiology, or how the diseases are caused, and how they spread in the brain.” While both conditions involve abnormal protein accumulation and progressive brain changes, the type of protein, and where it first appears, varies dramatically.
Where the Diseases Begin: Pathology and Progression
In Alzheimer’s disease, the core pathology centers around amyloid and tau. These proteins accumulate earliest in the brain’s memory structures. “We know Alzheimer's disease is caused by amyloid and tau deposition in different areas of the brain, mostly in the memory centers, and then it can spread cortically to different areas of the brain.”
In contrast, Parkinson’s disease is primarily driven by alpha-synuclein, the key component of Lewy bodies. This same pathology also appears in Lewy body dementia.
As Dr. Isaacson notes, “with Parkinson's… the deposition is with synuclein, which composes the Lewy body… present in Parkinson's disease as well.” Unlike Alzheimer’s, this synuclein pathology is believed to begin outside the brain. “This usually starts, we think, in the periphery and then spreads to different parts of the brain, including the basal ganglia that controls motor coordination, [and] different nuclei in the brainstem that controls blood pressure or mood.”
Because each disease targets different regions first, the earliest symptoms tend to differ as well.
How Cognition Differs Between Parkinson’s and Alzheimer’s
Memory loss is the defining early symptom of Alzheimer’s disease. This is tied directly to where amyloid and tau accumulate: “For Alzheimer's, the deposition typically is deposited in the hippocampus or other memory centers of the brain. So recall is a major issue with Alzheimer's.”
In Parkinson’s, memory problems usually develop later, and only in a subset of patients. “In Parkinson's disease, the cognitive onset is only in a small percentage of patients and it tends to be much later down the road.”
When cognitive changes do arise, they look different from classic Alzheimer’s memory impairment. “In Parkinson's, we see a lot of issues with attention, visuospatial, and concentration difficulties… that differs from the way Alzheimer's disease manifests itself.”
Parkinson’s cognitive symptoms also tend to fluctuate more throughout the day and often respond better to treatments used for memory support. “There's also much fluctuations with Parkinson's disease memory issues. And it tends to be much more responsive to different medications that's used for memory in Parkinson's disease.”
The Emerging Role of Biomarkers
Despite their distinct differences, Parkinson’s and Alzheimer’s also share overlaps, and in some cases, co-pathology. This has driven research into biomarkers that can help distinguish, predict, and track each condition.
Dr. Isaacson explains that “Parkinson's disease and Alzheimer's have a lot of overlap, and we also see a lot of co-pathology… So we're looking at different biomarkers that can overlay with both conditions.”
In Parkinson’s, synuclein is still central: “we tend to see more synuclein deposition… we can even start to detect synuclein in the blood.”
But other biomarkers traditionally associated with Alzheimer’s appear in Parkinson’s as well, especially those related to inflammation: “we see inflammation in the brain… we can see things like neurofilament light (NfL), or GFAP protein, being elevated at different points of the disease course.” These markers reflect cellular stress or inflammatory responses that evolve over time.
Tau, the hallmark Alzheimer’s protein, may also change in certain Parkinson’s presentations:
“We can sometimes see tau changes in Parkinson's disease, or other protein markers and other receptors that we didn't previously suspect were involved.”
Together, these markers offer a more nuanced picture of Parkinson’s subtypes, progression, and individual variability.
Studying Subtypes: The BioRAND Cohort
To better understand these differences, our researchers are turning to large-scale cohorts that examine how Parkinson’s behaves across diverse patients. Dr. Isaacson explains the goals of the BioRAND study and shares that, “we're trying to evolve that study to have a higher amount of patients… ‘Do different patients with Parkinson's disease behave differently?’”
These differences include genetics, family history, prodromal features, and symptom presentation, whether tremor, or cognitive, or gait problems.
Large cohorts are essential because Parkinson’s is highly heterogeneous. Dr. Isaacson notes that
“you really need a very high volume of patients to understand the disease course, of different subtypes of Parkinson's Disease.” Early findings from smaller groups show encouraging patterns, but scaling this work will allow researchers to determine how these subtypes differ over time, from the earliest prodromal periods to advanced stages.
As he emphasizes, “It's definitely an exciting time in better understanding each individual population.”
As the fields of Parkinson’s and Alzheimer’s research evolve, the distinctions, and overlaps, between the two conditions are becoming clearer. Advances in pathology, cognitive profiling, and biomarker development are making it possible to detect disease earlier, capture its heterogeneity, and tailor care to each patient’s biology. What once seemed like two distinct diseases now appear as part of a broader landscape of neurodegeneration, shaped by shared mechanisms but unique pathways.
This growing clarity offers tremendous hope. With deeper understanding comes the potential for earlier diagnosis, more precise treatments, and ultimately, interventions that may alter the course of these conditions. The future of neurodegenerative disease research is one of rising precision and growing possibility.
To learn more about biomarkers for Parkinson's and Alzheimer's diseases, watch our full conversation with Dr. Jonathan Isaacson in the video above.
By Alicia Barber Minteer, PhD
Disclaimer
The Video and Written Educational Content included on this site is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read or seen on the Site.
The information contained in the Educational Content posted represents the views and opinions of the individual in the recording and does not necessarily represent the views or opinions of IND. The mere appearance of Educational Content on the Site does not constitute an endorsement by IND or its affiliates of such Content.
The Educational Content has been made available for informational and educational purposes only. IND does not make any representation or warranties with respect to the accuracy, applicability, fitness, or completeness of the Content. IND does not warrant the performance, effectiveness or applicability of any sites listed or linked to in any Content. IND hereby disclaims any and all liability to any party for any direct, indirect, implied, punitive, special, incidental or other consequential damages arising directly or indirectly from any use of the Content, which is provided as is, and without warranties.