Research
Can we develop a new blood test for Brain Health?
Certain proteins found in the brain that are associated with Alzheimer’s disease (AD) and other neurodegenerative diseases (ND) can now be detected in the blood many years before the onset of symptoms. A study funded by donors to our Foundation is testing whether it is possible to detect these proteins in the blood of people with varying degrees of risk for AD and other diseases, including Parkinson’s disease (PD), Lewy Body Dementia (LBD) and Frontotemporal Dementia (FTD). The ability to monitor and track these protein markers in people before symptoms begin is critical for early detection and treatment.
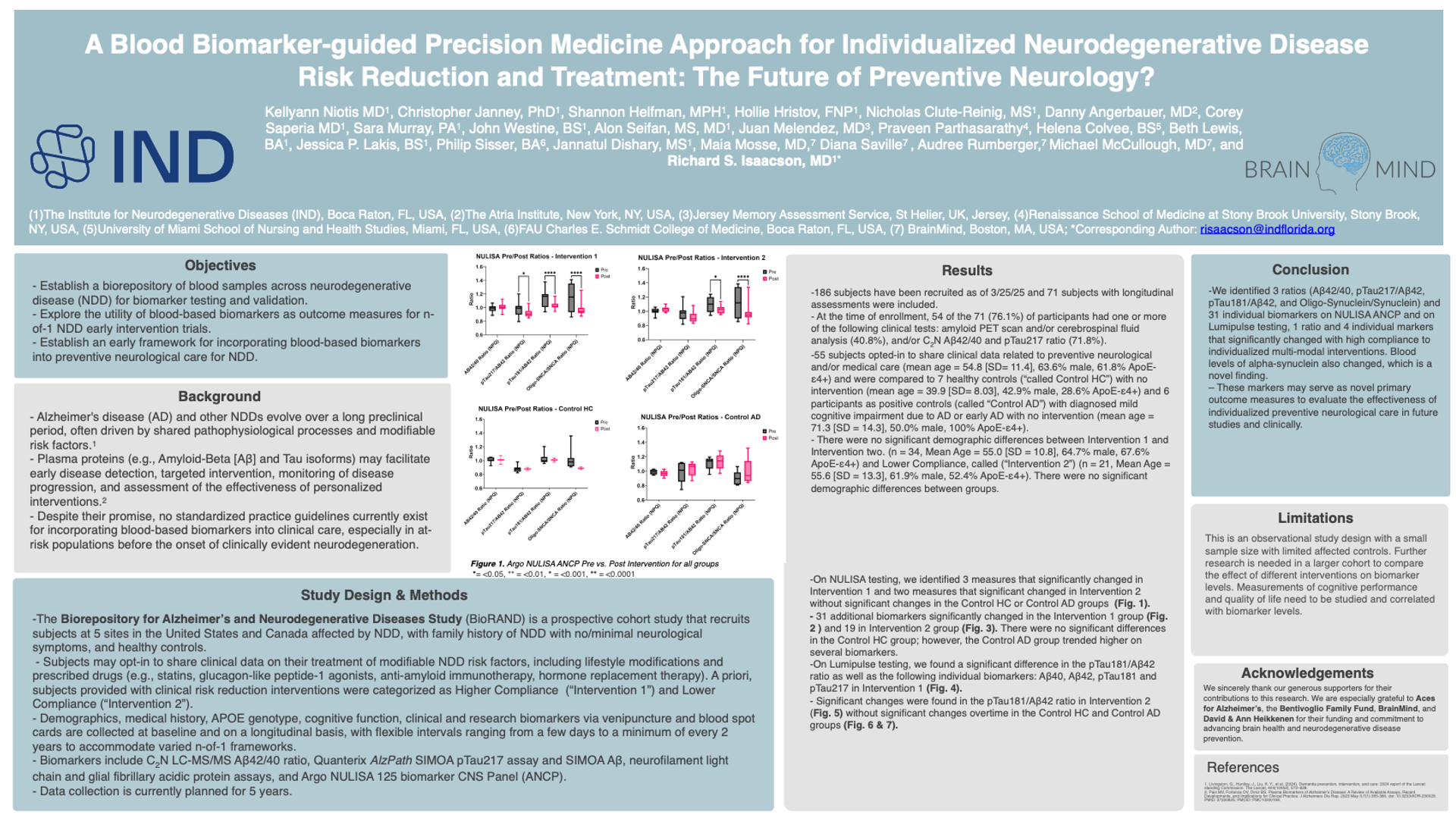
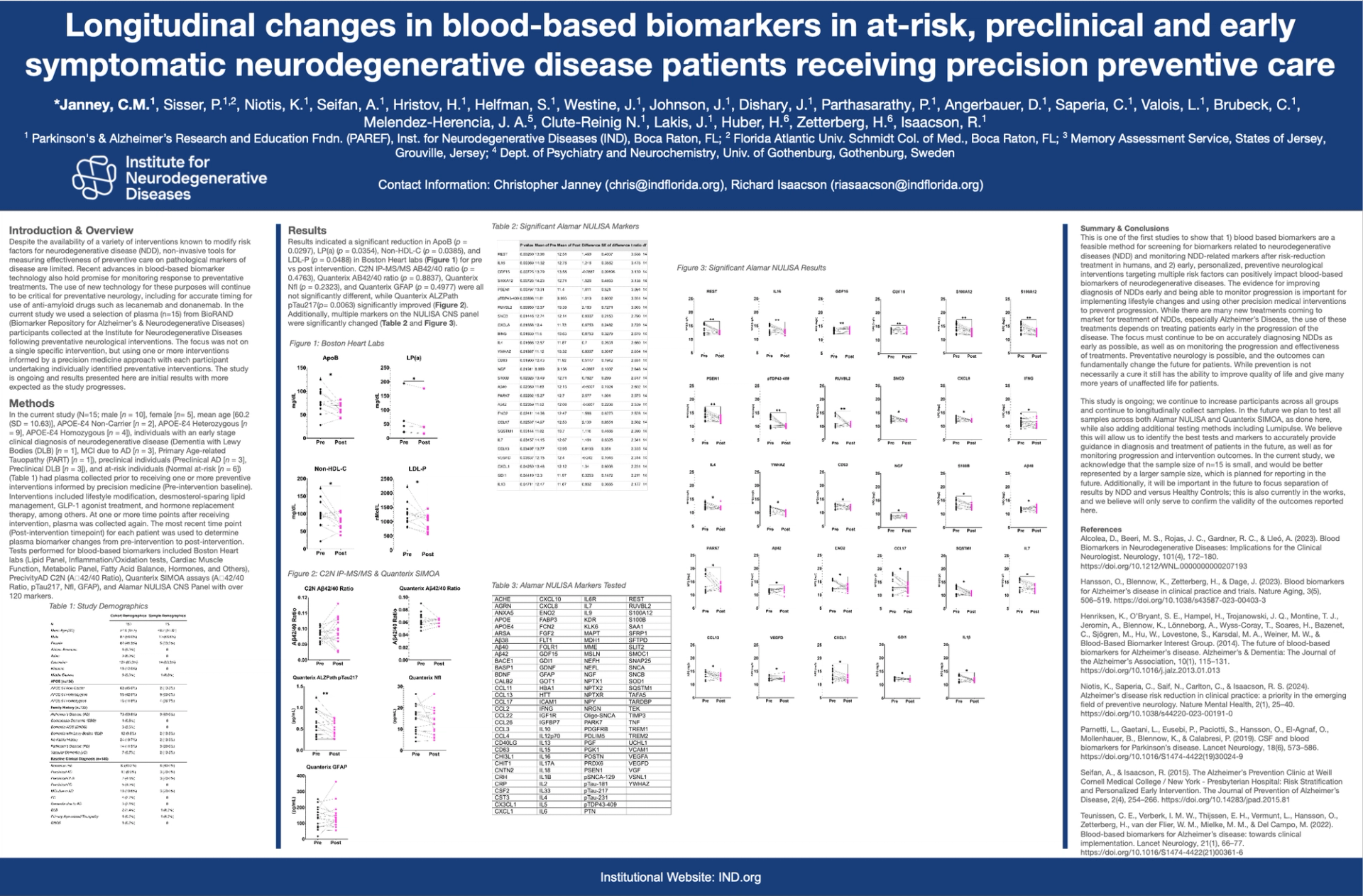
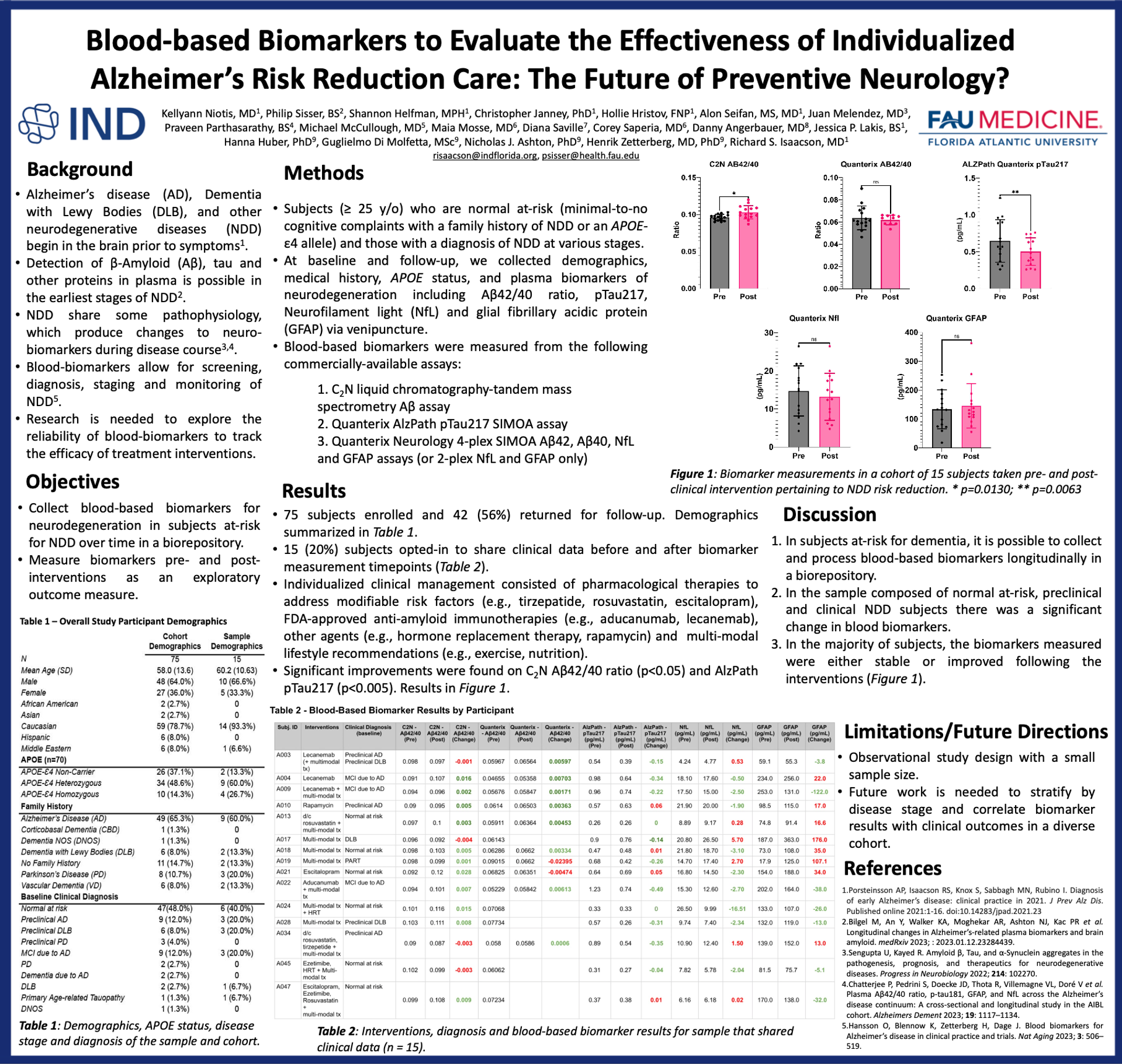
Just like when doctors suggest ways for people to lower their cholesterol (e.g., exercise, dietary changes, prescription drugs, or supplements) and then use cholesterol blood test values (like LDL, HDL and triglycerides) to assess the effectiveness of those interventions, our team is developing (as Dr. Richard Isaacson likes to say) a "cholesterol test for the brain". However, instead of looking at LDL, HDL and other cholesterol markers, we test for more than 120 novel brain proteins in our Boca Raton, FL laboratory. We can use these new tests to measure the effect of the risk reduction interventions that our participants may receive as part of their external clinical care. Our aim is to create tests that clinicans can use to evaluate the effectiveness of their interventions and then refine, or "fine-tune," a personalized treatment plan, ushering in the era of true personalized preventative brain health.
Our team has used observational “N-of-1” trials (or single participant studies) that consider an individual person when evaluating the effectiveness of different interventions on ND risk. Using the person as the sole unit of observation, the impact of various interventions, such as lifestyle changes (e.g., exercise, nutrition, stress reduction) as well as certain drugs, vitamins or supplements used for other medical conditions (e.g., diabetes, high cholesterol, peri-menopause, depression, high blood pressure), can be measured based on the change in blood-based markers of ND. Observing biomarkers both before and after various lifestyle and medical changes allows our research team to cost-effectively understand the biological impact of these interventions on AD and other ND pathology rather than by using tests that are riskier, more cumbersome, and costlier- such as lumbar punctures and brain imaging scans.
We have closed this study after enrolling 200 people whose cases we will continue to follow over time. Our cohort includes participants with a family history of, or with already diagnosed, AD, PD, LBD, or FTD, as well as control subjects. We are observing the effects of a variety of interventions provided by participants' treating clinicians. For example, we are tracking the effects of anti-amyloid drugs on patients with mild cognitive impairment due to Alzheimer's disease; cholesterol treatments on people at risk for ND or who are currently symptomatic; hormone replacement therapy in women; and multi-modal lifestyle risk reduction interventions such as exercise and dietary changes.
While Enrollment in this study is currently closed, we are actively looking for more funding to expand this work. We have presented initial findings on 75 participants at the 2024 American Academy of Neurology Meeting in Denver, CO, and the 2024 Alzheimer's Association International Conference in Philadelphia, PA. Stay tuned for more results and join our email Newsletter to stay in touch. Also, read our recent Blog Posts below or visit our Newsroom Page to learn more.
Precision Medicine & Genetics Research Program
A Foundation-supported research project focuses on the genetic factors that play a role in the development of AD and other ND. There are many genes – ranging from those that affect memory to those that affect cholesterol to sleep – that can impact the development of ND. It is our goal to be better able to acquire, store, and analyze whole genome sequencing, as well as partial genome sequencing, in people at risk for or already diagnosed with these conditions. We have enrolled several families and aim to study how genetic analyses may contribute to personalizing risk reduction care in a clinical research study.
Recent Publications
Can we determine Alzheimer’s disease neuropathology from the finger?
Inflammation biomarkers and Alzheimer’s disease: A pilot study using NULISAseq
Identify biological Alzheimer’s disease using a novel nucleic acid–linked protein immunoassay
Research Posters